Stop Snoring Surgery: What You Need to Know Before Going Under the Knife
Jun 26th 2023
Picture this: you're soaring through the sky, embracing the tranquility and sheer bliss of floating among clouds in your dream... only to be jolted out of sleep by that all-too-familiar chainsaw-like growl - snoring. It's not just ruining your sound slumber but is also driving your partner up the wall. But the question stands, have you ever thought about stop snoring surgery as a solution for peaceful nights? Before taking such a significant step, it’s crucial to know exactly what you might be diving into. Let's dissect the complexities and get a clear view before going under the knife.
There are several common types of surgery to address snoring, including Uvulopalatopharyngoplasty (UPPP), Maxillomandibular advancement (MMA), Hypoglossal nerve stimulation, and others. These surgeries work by addressing the underlying issues that cause snoring, such as airway obstruction or tongue muscle relaxation during sleep. It's important to consult with a qualified healthcare provider to determine which surgical option is best suited to your individual situation.
Understanding Snoring Surgery
Snoring can be a problematic issue for both those who snore and their partners. It can disrupt sleep quality and lead to daytime fatigue, irritability, and even depression. If you're experiencing severe snoring or obstructive sleep apnea that is not being helped by other treatment options, then surgical intervention may be necessary. While the decision to undergo surgery can be daunting, it's important to understand what's involved in the procedure before making any decisions.
Anecdotal evidence suggests that patients who opt for surgery have experienced life-changing results. However, it is essential to understand that every person's experience will be different. Some people may find relief from their symptoms while others may not see much improvement. Therefore, it's crucial to discuss the risks and benefits of surgery with your healthcare provider in advance.
Think of snoring as a puzzle with many pieces that all contribute to its onset. Addressing only one piece of the puzzle may not resolve the issue completely, which is why treating snoring can be challenging. While surgery can address some anatomical issues contributing to snoring, it is essential to consider the overall picture before rushing into making any decisions.
There are several factors to consider when deciding if snoring surgery is right for you. One critical factor to consider is whether other treatment methods or lifestyle changes have been effective in reducing snoring severity. Factors such as excess body weight, nasal congestion, sleeping position, and alcohol consumption can contribute to snoring episodes; thus taking corrective measures towards these factors should be exhausted first before considering surgery.
With an understanding of the considerations for determining if surgery is right for you now established let us dive deeper into the techniques used during the surgery process.
Anatomy Targeted in Surgery

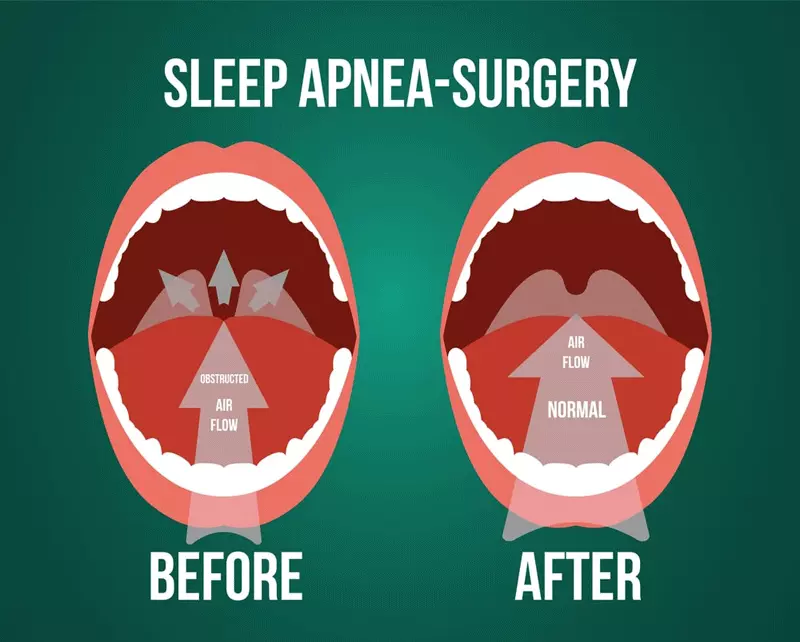
There are several muscles, tissues and bony structures within the mouth and throat that can cause snoring when they become relaxed or blocked. The surgical procedures target these specific anatomical areas to improve breathing quality and reduce the apnea during sleep. One of the key aspects of understanding snoring surgery is comprehending which areas are being targeted in each procedure.
Like a house with different rooms, there are many areas within the mouth and throat. Each procedure targets specific regions by removing, trimming or adjusting the tissue in one or more of these structures to create a successful airflow path through the airways.
In most patients, surgery for snoring will focus on the soft palate, uvula, tonsils, tongue base, and hypopharynx (lower part of the throat). These five structures play a crucial role in restricting airflow in people who snore. Removing a portion of these tissues can open up the airway space and improve snoring symptoms.
However, it's important to remember that snoring surgery isn't always a guaranteed solution for everyone struggling with the problem. Surgery should not be considered as an option unless other treatments have been unsuccessful or symptoms of sleep deprivation have become unmanageable.
A popular example among medical professionals is the pillar procedure; while this targets only one area in the mouth -the soft palate- it is frequently chosen due to its simple structure and perceived effectiveness. During this procedure small plastic rods are implanted into the soft palate where they provide structural support to reduce vibrations that cause snoring.
Weighing up the potential risks and rewards associated with each procedure can seem like an overwhelming task but knowledge about both aspects is necessary for determining if you think surgery might be worth considering.
Common Procedures Explained
There are various surgical procedures that snorers can undergo to alleviate their condition. These surgical options target different parts of the upper respiratory tract that are thought to contribute to snoring. Here are some of the most common procedures and how they work.
This procedure involves inserting small, slim plastic rods into the soft palate at the back of your mouth. The pillars are aimed at stiffening the soft palate and preventing it from collapsing on itself during sleep, which can cause snoring. Patients often report less frequent snoring and improved sleep quality after having this procedure performed.
This surgery removes excess tissue in the uvula, tonsils, and soft palate to widen the airway. UPPP is a complex surgery that is more invasive than some other procedures and may require a hospital stay. It is typically recommended for severe cases of obstructive sleep apnea that haven't responded to other treatments.
RFA and LAUP are relatively non-invasive treatments for snoring that aim to reduce or eliminate the amount of tissue that vibrates during sleep in the throat area. The procedures involve using heat from radio waves or lasers to shrink or remove excess tissue from the uvula or soft palate. In general, RFA and LAUP are less effective than UPPP or more invasive procedures.
MMA is a type of orthognathic (jaw) surgery designed to correct moderate-to-severe obstructive sleep apnea by moving both the upper jaw (maxilla) and lower jaw (mandible) forward. By advancing both jaws simultaneously, patients tend to experience immediate improvement in breathing as the airway opening becomes larger.
This is a newer procedure that involves the insertion of an implantable device under the skin below the collarbone. The device senses when a snorer stops breathing or starts to gasp for air and then sends an electrical signal to the hypoglossal nerve to stimulate the tongue muscles and increase breathing. Studies have shown promising results with this procedure, and it may become more widely available in the future.
These procedures are performed on the nose to relieve nasal obstruction and improve airflow. Septoplasty refers to surgery that straightens a deviated septum while turbinate reduction shrinks the size of turbinates which aid in humidification and filtration of incoming air. When these obstructions are removed, patients may experience less snoring.
This surgical option involves repositioning the muscle attached to the bottom of your tongue in a way that prevents it from falling back into your throat during sleep. By pulling the tongue forward, the airway opening is increased so patients can breathe more easily.
This procedure stabilizes and suspends the hyoid bone at the front of your neck, which controls several important throat muscles involved in breathing. By surgically securing this bone in place, it can prevent the throat from collapsing during sleep, which can minimize snoring.
To sum up, each surgical procedure has its unique benefits and challenges. Choosing between them requires careful consideration of factors such as medical history, individual anatomy, and lifestyle habits (such as use of alcohol or tobacco) to ensure maximum patient outcomes. In many cases, a healthcare professional works together with a specialist center such as an oral surgeon or sleep medicine physician to create personalized treatment plans based on individuals' specific needs.
Weighing the Pros and Cons
If you're considering snoring surgery, it's important to understand the potential risks and rewards. Here are some key factors to consider before making a decision.
Potential Benefits
- Reduced snoring and improved sleep quality for patients
- Improved breathing ability during sleep, which can benefit overall health
Potential Risks
- As with any surgery, there is always the risk of complications such as bleeding, infection, or reactive airway disease.
- Most surgeries require anesthesia, which carries its own risks.
- In some cases, snoring may return several years after surgery due to the progression of age-related tissue loss.
Making a Decision
It's essential to weigh both the benefits and risks before making a decision about surgery. For some people with severe snoring or obstructive sleep apnea, surgery may be an effective option when other treatments have failed. However, others may find that the potential risks outweigh the benefits.
As with any health decision, it's essential to consult your healthcare provider and discuss your specific case thoroughly. They can help you understand the details of different procedures and determine whether they may be right for you.
Think of it like buying a car: there is no single "best" choice - each model has its unique features and benefits. Some models might prioritize efficiency over horsepower while others might focus more on style. Similarly, surgical options treat various aspects and causes of snoring - what might work best for one individual is not necessarily going to be right for everyone else. Ultimately, it is up to you in consultation with your healthcare provider to choose what feels most suitable concerning medical history, physical needs as well as personal preferences (including timing).
While surgery can lead to significant improvement in snoring conditions and better quality of life outcomes for many patients, it is essential also to gain a thorough understanding of alternative treatments that could effectively provide support without involving surgery. In the next section, we will discuss the effectiveness of these alternative treatments relative to surgical interventions.
Potential Risks and Rewards
When it comes to snoring surgery, it is essential to understand both the potential benefits and drawbacks of such procedures. On one hand, surgery can offer lasting relief for those who struggle with snoring and sleep apnea. On the other hand, it is not without its risks, and there is no guarantee that it will be successful for everyone.
One of the most significant advantages of snoring surgery is that it can lead to a better night's sleep. Chronic snoring or sleep apnea often leads to poor sleep quality due to frequent waking up during the night. This can cause daytime fatigue, difficulty concentrating, and other issues, impacting a person's daily life. For some individuals, surgery can bring about significant improvements in their ability to breathe through their nose while sleeping, leading to deeper, more restful sleep.
Another potential benefit of snoring surgery is an improvement in overall health. Sleep apnea has been linked to a higher risk of heart disease and stroke. While not all cases of snoring are related to sleep apnea, addressing the underlying issue may reduce the risk of these serious conditions.
However, as with any surgical procedure, there are risks involved. Snoring surgery can result in complications such as pain, bleeding, swelling or infection after the procedure. In rare cases, patients may also experience anesthesia-related risks or respiratory complications after surgery. It is important to fully discuss these risks with your doctor before making a decision about whether surgery is right for you.
Comparing any surgical decision to buying a house isn't ideal, but weighing costs against potential benefits work similarly. Just like buying a house has financial risks involved; there are definitely some physiological ones associated with snoring surgery as mentioned above on top of that in some instances like UPPP procedure, there is a 60% success rate among patients. To ensure you are making the right decision for your overall health, it's essential to weigh all of the factors in reflection.
- Studies suggest that more than 60% of people who undergo palatal implant surgery (pillar procedure) for snoring have a significant reduction in snoring intensity.
- The American Sleep Association states that uvulopalatopharyngoplasty (UPPP), a common surgical method to combat severe snoring, has a success rate between 40% and 60%.
- According to a clinical trial reported in British Medical Journal, patients who underwent hypoglossal nerve stimulation saw an average reduction of 70% in their apnea-hypopnea index (AHI), a measure of sleep apnea severity.
Surgical Procedures Versus Alternatives
If you're considering surgery as an option to alleviate snoring, it is important to know what alternatives may be available. While surgery can be effective for severe cases of snoring, there are also other treatments that may be less invasive and could be worth trying first.
One potential non-surgical option is lifestyle changes such as weight loss or reducing alcohol consumption before bedtime. For some individuals, these adjustments may significantly reduce or even eliminate snoring altogether. It's worth noting that these methods tend to work better for mild cases of snoring and may not be as effective for those with more sever sleep apnea issues.

Oral appliances like the Zyppah mouthpiece can also be quite effective at reducing snoring. These devices work by slightly shifting the position of the jaw during sleep, helping to prevent airway blockages that cause snoring. With a high success rate (88% of users report reduced snoring), many individuals find them to be an excellent alternative to surgery.

In some cases, nasal strips or decongestants can also help with congestion and enable individuals to breathe easier at night. Additionally, CPAP machines provide continuous oxygen flow while sleeping and have a 100% success rate at treating sleep apnea; however, they can be difficult to get used due its cumbersome headgear.

While these options often show good results for some SNORING situations, they aren't always appropriate for the management of obstructive sleep apnea (OSA). After all provisions have been exhausted without success; then surgical procedures become a suitable approach. An ENT(ear, nose, throat) doctor can guide patients to the right surgical procedure that is befitting to their sleeping disorder.
Like every aspect of life, there's a risk versus reward advantage with every decision. Before moving towards more invasive options for snoring issues like surgery, it's always advisable to explore less risky options like lifestyle changes, mouthpieces, and other non-surgical procedures first. Taking this approach will either resolve the snoring issue or provide relief through the less invasive methods without undergoing surgical interventions.
Comparison of Effectiveness
If you're considering snoring surgery, it's important to weigh the pros and cons of each procedure. While all surgeries come with some risks, some procedures may be more effective than others in treating your specific case of snoring.
One commonly used procedure is the pillar procedure or palatal implant. This involves inserting small polyester rods into the soft palate to stiffen it and reduce vibrations that cause snoring. While this procedure has shown some success in reducing snoring, studies have also shown a high rate of implant extrusion or failure.
Another surgical option is Uvulopalatopharyngoplasty (UPPP), which involves removing excess tissue in the throat and soft palate to widen the airway and reduce snoring. Although UPPP has been effective for some patients, it is a more invasive procedure that requires general anesthesia and can result in a long and painful recovery period.
Radiofrequency ablation and laser-assisted uvulopalatoplasty are minimally invasive procedures that use heat to remove tissue from the back of the throat. These procedures can be effective in reducing snoring for some patients but are not recommended for those with sleep apnea.
Maxillomandibular advancement (MMA) involves moving the upper and lower jaws forward to open up the airway, which can be helpful for those with severe sleep apnea. However, this is a major surgery that requires a longer recovery time and has a higher risk of complications.
Lastly, hypoglossal nerve stimulation involves implanting a device under the skin that stimulates nerves controlling tongue movement. This helps keep the airway open during sleep, reducing snoring and improving breathing for those with moderate to severe sleep apnea.
Ultimately, no single procedure will work for everyone. Each person’s anatomy is unique, so it’s important to consult with a doctor before undergoing any of these procedures. A sleep study may be necessary to determine the underlying cause of your snoring and which procedure may be the most effective for you.
Deciding If Snoring Surgery is Right for You
If you’re considering snoring surgery, it’s important to carefully consider all your options. While surgery can be effective in treating certain types of snoring, there are also risks and potential complications involved. Here are a few things to keep in mind when deciding if snoring surgery is right for you:
Think of snoring surgery like any other surgical procedure. It’s important to weigh the benefits and risks associated with the procedure against the impact that your snoring is having on your quality of life. For some people, snoring may be more of a nuisance than anything else. In those cases, lifestyle changes or minimally invasive treatments may be a better option. However, if your snoring is causing serious problems, such as poor sleep quality or sleep apnea, surgery may be worth considering.
Keep in mind that no surgical procedure is without risk. Complications from anesthesia, bleeding, infection, or nerve damage can occur during any surgery. It’s important to discuss potential risks with your doctor and consider the likelihood and severity of any potential complications.
Additionally, snoring surgery requires a recovery period during which pain, discomfort and restrictions on activity are common. Make sure you have support from friends and family while you recover from any procedure.
Before making a decision about whether or not to undergo snoring surgery, consider trying non-surgical treatment options such as positional therapy devices or oral appliances first. These options can often improve airflow during sleep without requiring invasive procedures.
Ultimately, the decision to undergo snoring surgery is a personal one that should be based on your individual circumstances and needs. Consult with a doctor who specializes in snoring and sleep disorders to discuss options for treatment. With some research and thoughtful consideration, you can make an informed decision that improves your sleep and quality of life.
- Snoring surgery can be effective for treating certain types of snoring, but it's important to carefully weigh the benefits and risks. No surgical procedure is without risk, and there is a recovery period during which pain, discomfort, and activity restrictions are common. Before considering surgery, try non-surgical treatment options such as positional therapy devices or oral appliances. Ultimately, the decision to undergo snoring surgery should be based on individual circumstances and needs and made in consultation with a doctor who specializes in snoring and sleep disorders.
Answers to Commonly Asked Questions
How effective is stop snoring surgery at treating snoring?
Stop snoring surgery can be an effective solution for treating snoring, but it's important to note that its success rate varies depending on the type of surgery and the patient's individual case. In general, surgical procedures have been shown to significantly improve snoring symptoms in roughly 70-85% of cases.
However, it's also worth mentioning that surgery isn't always necessary or appropriate for every snoring sufferer. Before considering surgery, patients should exhaust all non-surgical options such as lifestyle changes or oral appliances that may reduce snoring symptoms.
Additionally, any surgery - including stop snoring procedures - comes with potential risks and complications. Patients should carefully weigh the benefits and risks before deciding on a surgical option and consult with their healthcare provider to fully understand the procedure and its potential outcomes.
Overall, while stop snoring surgery can be highly effective for many people, it's not a one-size-fits-all solution and should be considered thoughtfully alongside other treatment options.
Are there any alternative treatments for snoring besides surgery?
Yes, there are alternative treatments for snoring besides surgery. In fact, surgery should be considered as a last resort after trying out non-invasive options first.
One of the most effective non-surgical treatments is Continuous Positive Airway Pressure (CPAP) therapy, which involves wearing a mask that delivers pressurized air to keep the airway open during sleep. According to a study published in the Journal of Clinical Sleep Medicine, CPAP therapy has been found to significantly reduce snoring and improve quality of life for patients with sleep apnea.
Additionally, lifestyle changes such as weight loss, avoiding alcohol before bedtime, and sleeping on your side instead of your back have also been shown to be effective in reducing snoring. A study published in the journal Chest found that overweight individuals who lost just 10% of their body weight saw a significant decrease in their snoring.
Other non-surgical treatments include oral appliances that reposition the jaw to help keep the airway open, nasal strips that help improve nasal breathing, and positional therapy devices that prevent individuals from sleeping on their backs.
Overall, it is important to explore all non-surgical options before considering surgery for snoring. Not only are these alternatives less invasive and costly, but they have also been proven to be effective in improving sleep quality and reducing the risks associated with sleep apnea.
What are the potential risks and complications associated with stop snoring surgery?
Stop snoring surgery can be an effective solution for people who suffer from obstructive sleep apnea (OSA) or chronic snoring. However, like any surgical procedure, there are potential risks and complications that patients need to be aware of before going under the knife.
According to a study published in the American Journal of Otolaryngology-Head and Neck Medicine, the most common complications associated with stop snoring surgery include bleeding, swelling, and infection. These can occur in up to 5% of cases and may require additional medical treatment.
Another potential risk is damage to surrounding structures such as the tongue, teeth, or uvula. This can cause difficulty swallowing, speech problems, or even partial or complete loss of these structures.
In addition to physical complications, there are also psychological risks associated with stop snoring surgery. Some patients may experience anxiety, depression, or dissatisfaction with the results of the procedure.
It's important for patients to thoroughly discuss all potential risks and complications with their surgeon prior to undergoing stop snoring surgery. They should also carefully weigh the benefits against the risks and consider non-surgical options such as lifestyle changes or using a continuous positive airway pressure (CPAP) machine.
In conclusion, while stop snoring surgery can greatly improve quality of life for some individuals with OSA or chronic snoring, it is not without risk. Patients should educate themselves on the potential complications and make an informed decision with their healthcare provider.
What types of surgeries are available to treat snoring?
If you're one of the many individuals who feels like they're sawing logs throughout the night, you might be contemplating undergoing surgery to put an end to your snoring for good. Fortunately, several types of surgeries are available depending on your specific needs and preferences.
The most common type of surgical procedure for snoring is uvulopalatopharyngoplasty (UPPP), which involves removing excess tissue from the throat and palate to widen the airway. UPPP has been successful in decreasing snoring in roughly 65% of patients, according to research published in the Journal of Otolaryngology-Head & Neck Surgery.
Another option is nasal surgery, which generally focuses on correcting nasal obstruction issues that may contribute to snoring. Procedures such as septoplasty and turbinate reduction can help improve breathing and reduce snoring by increasing airflow through the nose.
Additionally, newer, more innovative techniques include laser-assisted uvulopalatoplasty (LAUP) and radiofrequency ablation (RFA), which use heat energy to decrease or eliminate excess tissue in the throat and reduce snoring. While these procedures are still relatively new compared to traditional surgeries like UPPP, research has shown them to be effective in treating some cases of snoring.
It's essential to recognize that surgery isn't always a guarantee for a permanent cure for snoring and may even come with potential risks and complications. As always, it's crucial to consult with a qualified medical professional before making any decisions about surgical procedures.
In conclusion, several types of surgeries can help treat snoring, including UPPP, nasal surgery, LAUP, and RFA. However, individual results can vary based on factors like the severity of snoring and overall health condition. Therefore, it's always important to consult with a medical professional before considering any form of surgical intervention.
What factors should be considered when deciding if stop snoring surgery is the right option?
Before considering stop snoring surgery, several factors should be taken into account. Firstly, it is important to know the cause of your snoring. Snoring can be caused by several factors such as obesity, alcohol consumption, nasal congestion or sleep apnea. It is vital to work with your doctor in order to determine the underlying cause and whether or not surgery is a suitable option.
Another factor to consider is the effectiveness of the surgery for addressing your condition. Despite its high success rate for treating obstructive sleep apnea (OSA), other types of snoring may not be cured by surgery alone. Research has shown that non-OSA related snoring had higher relapse rates after surgery compared to patients with OSA related snoring (1).
Additionally, one must also evaluate the risks involved with any form of surgical procedure along with the recovery time required post-surgery. Some procedures carry more risks than others. For example, uvulopalatopharyngoplasty (UPPP) has been shown to have high morbidity and complications rate due to the intricacy of the procedure
(2).
Lastly, one should assess the potential cost of surgery and whether it fits their budget. While insurance may cover some procedures, others may require out-of-pocket expenses that can significantly impact overall costs.
In conclusion, considering all these factors before going under the knife for stop snoring surgery is crucial for making an informed decision about which type of surgery is right for you, if any.
References:
1) J Jin et al., “Efficacy of multiple-level arterial muscle-paring palatopharyngoplasty depending on locations and severity of airway collapse in Obstructive Sleep Apnea,” Scientific Reports 11, no. 1 (2021): 6476.
2) Park et al., “Surgical Management of Snoring: Uvulopalatal Flap” Journal of Craniofacial Surgery 28, no.4 (2017): e347-e352.
