Tonsillectomy for Sleep Apnea: Surgery and Recovery Process
Aug 20th 2023
Experiencing incessant sleepless nights due to sleep apnea can make you feel like you're fighting an invisible battle. If countless sleep aids, medications, or lifestyle changes have proven ineffective, perhaps it's time to consider a more permanent solution: a tonsillectomy. This age-old surgical procedure could be your ticket to peaceful slumber and increased daytime energy. In this blog post, we'll delve deep into what a tonsillectomy entails for those suffering from sleep apnea — from the actual surgery to the recovery process — bringing you one step closer to truly restful nights.
Yes, tonsillectomy can be an effective treatment for sleep apnea in some cases, particularly in children with enlarged tonsils. Studies have shown a significant decrease in the average apnea-hypopnea index after tonsillectomy alone in adults with marked enlargement of the tonsils and sleep apnea. However, it is not considered a first-line treatment in adults due to several factors, and personalized medicine and individual patient circumstances should always be considered when making treatment decisions. As with any surgical procedure, it's important to consult with an ENT specialist to determine if tonsillectomy is the right option for you.
Understanding Sleep Apnea

Sleep apnea is a common sleep disorder affecting millions worldwide. It is characterized by pauses in breathing or shallow breaths during sleep, leading to disrupted sleep patterns and inadequate oxygen supply to the body. Understanding the basics of sleep apnea can help individuals recognize its symptoms and seek appropriate treatment.
There are three main types of sleep apnea: obstructive sleep apnea (OSA), central sleep apnea (CSA), and complex or mixed sleep apnea. OSA is the most prevalent form and occurs when the throat muscles relax, causing a blockage in the airway. Conversely, CSA happens when the brain fails to send proper signals to the muscles responsible for breathing. Complex or mixed sleep apnea combines both obstructive and central components.
Sleep apnea can have various causes ranging from structural issues such as enlarged tonsils or obesity to underlying medical conditions like hypothyroidism or congestive heart failure. It is essential to consult with a healthcare professional for a thorough evaluation if you suspect you may have sleep apnea.
Sarah, a 45-year-old woman who has struggled with loud snoring and excessive daytime fatigue, sought medical attention after her partner noticed episodes where she briefly stopped breathing during sleep. Her doctor diagnosed her with obstructive sleep apnea caused by enlarged tonsils and recommended further investigation.
Investigating further into the condition involves undergoing specific tests, such as polysomnography, which monitors brain activity, eye movements, heart rate, and breathing patterns during sleep. This data helps healthcare professionals make an accurate diagnosis and determine an appropriate treatment plan.
Now that we have better understood sleep apnea, let us move on to recognizing its symptoms.
- Sleep apnea is a common sleep disorder affecting millions worldwide. It can have various causes and has three primary types: obstructive, central, and complex. It is important to consult with a healthcare professional if you suspect you may have sleep apnea. A diagnosis involves specific tests such as polysomnography. Recognizing the symptoms of sleep apnea can help individuals seek appropriate treatment.
Recognizing The Symptoms
Recognizing sleep apnea symptoms is crucial for early diagnosis and intervention. While its common to experience occasional snoring or brief pauses in breathing during sleep, consistent symptoms should raise concerns. Some key indicators of sleep apnea include:
Loud and persistent snoring: Snoring alone does not always indicate sleep apnea, but it is a prevalent symptom among those with the disorder. The intensity and duration of snoring can vary, so it's important to pay attention to other accompanying symptoms.
Pauses in breathing: Brief interruptions in breathing, often followed by gasping or choking sounds, can be indicative of sleep apnea. These interruptions disrupt the quality of sleep and may go unnoticed without a bed partner or witness.
Excessive daytime sleepiness: Feeling excessively tired during the day, even after a full night's rest, can be a significant sign of sleep apnea. Individuals may struggle to stay awake while performing routine tasks or experience difficulty concentrating.
Fatigue and morning headaches: Waking up feeling tired and experiencing frequent headaches upon awakening are signs that your sleep is being disrupted throughout the night.
Dry mouth and sore throat: Breathing through the mouth while asleep can result in a dry mouth or sore throat in the morning. This occurs due to inadequate airflow during sleep.
It’s important to note that these symptoms can vary between individuals, and not everyone experiences all of them. If you suspect you may have sleep apnea based on these signs, it's essential to consult with a healthcare professional who can conduct proper testing and provide an accurate diagnosis.
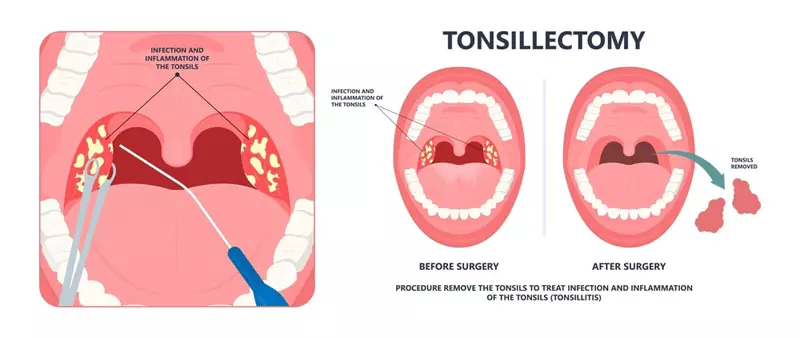
Surgical Solution: Tonsillectomy
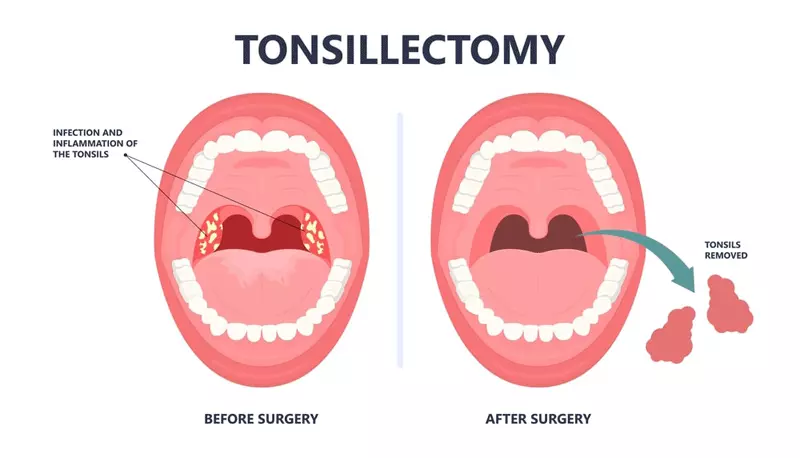
Tonsillectomy, a surgical procedure involving the removal of the tonsils, is considered a potential solution for individuals suffering from obstructive sleep apnea (OSA). The tonsils play a role in OSA by contributing to airway obstruction during sleep. By removing the tonsils, it aims to alleviate the symptoms and improve sleep quality for those affected.
The procedure is typically performed under general anesthesia and involves completely removing the tonsils. In some cases, additional procedures like adenoidectomy (removal of the adenoids) may be performed simultaneously.
Tonsillectomy for sleep apnea can bring significant benefits, such as reducing or eliminating snoring, improving airflow during sleep, and minimizing episodes of breathing pauses. This can ultimately lead to better overall sleep quality and improved daytime functioning.
However, its important to note that not all individuals with OSA will benefit from tonsillectomies. The suitability of this procedure depends on several factors, including the underlying cause of their sleep apnea, age, medical history, and individual circumstances. A thorough evaluation by a qualified healthcare professional is crucial in determining whether a tonsillectomy is appropriate.
Now that we understand the primary purpose of a tonsillectomy in addressing sleep apnea let's explore the risks and rewards associated with this surgical procedure.
Procedure Risks and Rewards
Every medical procedure carries its risks and rewards, and a tonsillectomy is no exception. It’s vital for patients considering this surgery to have a comprehensive understanding of what they might encounter along their journey toward improved sleep health.
One of the potential risks associated with a tonsillectomy includes bleeding during or after surgery. While this risk is generally low, it does exist. Patients are typically advised on specific precautions, such as avoiding certain medications that may increase the likelihood of bleeding and being mindful of physical activities that could strain the surgical site.
Let’s imagine a patient named Sarah who underwent a tonsillectomy for sleep apnea. In her case, she experienced some post-operative bleeding during the first few days. However, she followed her healthcare provider’s instructions, sought prompt medical attention, and ultimately fully recovered.
Aside from bleeding, other risks include infection, adverse reactions to anesthesia, and potential changes in voice or swallowing. These risks are relatively rare but should be discussed with the surgical team beforehand.
Conversely, tonsillectomy can offer significant rewards for individuals experiencing sleep apnea symptoms. It has been found to reduce or eliminate snoring and improve airflow during sleep effectively. This can result in better overall sleep quality, reduced daytime sleepiness, improved cognitive function, and improved quality of life.
While it’s important to be aware of the potential risks associated with tonsillectomy for sleep apnea, it’s equally essential to consider the individual rewards this procedure can bring. Understanding both sides will empower patients to make informed decisions regarding their treatment options.
- Research indicates that in children with Obstructive Sleep Apnea Syndrome (OSAS), nearly 80% experienced improvement or total resolution of the syndrome following a tonsillectomy and adenoidectomy.
- A study conducted on 29 adults who underwent tonsillectomy as a treatment for sleep apnea showed a significant decrease in average apnea-hypopnea index from 40 to 7 events per hour post-surgery.
- Post-tonsillectomy, young adults with markedly enlarged tonsils struggling with Positive Airway Pressure therapy have over a 90% chance of easing their sleep apnea symptoms, according to professionals advocating for personalized medicine and tailored approaches to sleep apnea treatment.
Post-Surgery: Recovery and Complications
After undergoing a tonsillectomy for sleep apnea, the recovery process becomes crucial for success. While each individual’s experience may vary, knowing the general factors affecting recovery and potential complications is important. Proper post-surgery care and understanding of potential issues can help navigate this period more smoothly.
During the first few days following the surgery, it is common to experience moderate to severe throat pain and discomfort in the ears, neck, or jaw. This discomfort can make swallowing difficult and may result in reduced appetite. Additionally, individuals might also experience nausea and vomiting due to the effects of anesthesia and the healing process.
Take Samantha, a 32-year-old who recently underwent a tonsillectomy to treat her sleep apnea. She describes her post-surgery experience as incredibly painful. Her throat was raw and tender, making it challenging to eat even small portions of food. The discomfort in her ears and neck added an extra layer, making her recovery more challenging.
Moreover, mild fever might be present during this time, which is a normal response by the body to surgical trauma. Bad breath is another common occurrence due to the healing process in the throat area. The tongue or throat might also swell temporarily, causing temporary difficulty in speaking or breathing.
Sometimes, individuals might feel something stuck in their throat after the surgery. It’s important not to panic if this sensation arises; it usually subsides as the healing progresses. However, if any concerns persist or worsen during recovery, it is important to consult with your healthcare provider promptly.
Now that we have discussed some of the typical post-surgery experiences one may encounter during recovery from a tonsillectomy for sleep apnea, let’s explore steps towards recovery and potential complications.
Steps Towards Recovery and Potential Complications
To ensure a smooth recovery and minimize the risk of complications, there are several steps individuals should take after undergoing a tonsillectomy for sleep apnea. These steps focus on managing pain, promoting healing, and recognizing potential red flags that require immediate medical attention.
The first step is to follow the prescribed pain medication regimen as directed by your healthcare provider. Taking pain medications regularly can help alleviate the discomfort and allow for better rest during the recovery period.
Ensuring adequate fluid intake is crucial to avoid dehydration. Drinking plenty of fluids is vital during this time, especially if eating solid foods proves challenging. Opting for cold or lukewarm liquids can provide soothing relief to the throat.
When it comes to nutrition, starting with bland foods that are easy to swallow is recommended initially. Gradually introducing more textured and flavorful foods as tolerated can help ensure proper nutrition while avoiding any unnecessary strain on the healing area.
Resting is essential for allowing the body to recover effectively. Taking time off from work or school and avoiding strenuous physical activities for at least two weeks can aid in the healing process and reduce the risk of complications.
Recovery from a tonsillectomy can be compared to recovering from a marathon—both require adequate rest, nourishment, and patience as the body heals.
While most individuals experience an uneventful recovery, it's important to remain vigilant for potential complications that require prompt medical attention. These may include:
- Bleeding: If bright red blood is noticed in the throat or excessive bleeding occurs, it is crucial to seek immediate medical care.
- Fever: A fever of 102°F (38.9°C) or higher could indicate an infection or other complications.
- Dehydration: Reduced urination, extreme thirst, and dizziness can be signs of dehydration, which requires medical attention.
- Breathing problems: If there is difficulty breathing or any other respiratory distress, it should be addressed promptly.
By following these steps and being aware of potential complications, individuals can take an active role in their recovery journey and ensure a successful outcome from their tonsillectomy for sleep apnea.
Ensuring a Successful Treatment

When considering a tonsillectomy as a treatment for sleep apnea, certain factors contribute to ensuring its success. One crucial aspect is selecting the right specialist and undergoing proper follow-up care.
It’s essential to find a highly experienced surgeon specializing in sleep apnea with a strong track record of successful tonsillectomies. Look for a doctor who is board-certified in otolaryngology or head and neck surgery, as they possess the necessary expertise in dealing with upper airway conditions, including the removal of tonsils.
Once you have found a potential specialist, schedule an initial consultation to discuss your case. During this consultation, the surgeon will evaluate your specific situation, including the severity of your sleep apnea and any other relevant medical conditions. They will also review your medical history and may order further tests or evaluations, such as a sleep study, to gather more information.
Let’s say you schedule a consultation with Dr. Smith, who has extensive experience in performing tonsillectomies for patients with sleep apnea. During the visit, Dr. Smith thoroughly examines and reviews your medical records, including reports from previous sleep studies. Based on their expertise and evaluation, Dr. Smith confirms that you are a suitable candidate for a tonsillectomy to treat your sleep apnea.
Once you have chosen the right specialist for your tonsillectomy procedure, it is important to follow up with post-operative care diligently. Your surgeon will provide specific instructions regarding diet restrictions, pain management techniques, and when to come in for follow-up appointments.
Now that we understand the importance of choosing the right specialist and following up properly after tonsillectomy surgery let’s explore how to make these critical decisions.
Choosing the Right Specialist and Follow-Up Care

Choosing the right specialist for your tonsillectomy is vital to the success of your treatment. Look for a surgeon who has expertise in sleep apnea surgeries and demonstrates excellent communication skills and a willingness to address your concerns. It’s important that you feel comfortable and confident with your chosen specialist throughout the entire process.
Finding recommendations from trusted sources such as friends, family, or your primary care physician can be a good starting point in identifying potential specialists. Additionally, you can research online to read reviews and testimonials from other patients who have undergone similar procedures.
When selecting a specialist, it’s crucial to consider their experience and track record. Look for board certification in otolaryngology or head and neck surgery and inquire about their specific experience with tonsillectomies for sleep apnea. Ask how many such procedures they have performed, their success rates, and whether they have encountered any complications.
Besides choosing the right specialist, follow-up care is equally important for a successful recovery. Your surgeon will provide detailed post-operative instructions that should be followed diligently. This may include information on pain management, diet restrictions, oral hygiene practices, and when to schedule follow-up appointments.
Some patients may find it tempting to downplay the significance of certain follow-up appointments or disregard post-operative instructions due to inconvenience or discomfort. However, it’s crucial to understand that these measures are implemented to ensure proper healing and minimize complications during your recovery period. Deviating from the prescribed post-operative care plan can potentially compromise the success of your treatment.
By selecting the right specialist and closely adhering to post-operative care instructions, you significantly increase the chances of a successful tonsillectomy procedure for sleep apnea treatment.
How common is tonsillectomy as a treatment for sleep apnea?
Tonsillectomy is a common treatment for sleep apnea, especially in children. According to the American Academy of Otolaryngology-Head and Neck Surgery, around 80% of children with obstructive sleep apnea have enlarged tonsils as the primary cause, making tonsillectomy an effective solution. In adults, while it is less common compared to other treatments like continuous positive airway pressure (CPAP), tonsillectomy may be recommended in certain cases where enlarged tonsils are contributing to sleep apnea symptoms.
Are there any alternative treatments for sleep apnea besides tonsillectomy?
there are alternative sleep apnea treatments besides tonsillectomy. Continuous positive airway pressure (CPAP) is the most common non-surgical treatment, where a machine delivers air pressure through a mask to keep the airways open during sleep. Other options include oral appliances, which position the jaw and tongue to improve airflow, and lifestyle changes like weight loss and avoiding alcohol and sedatives. According to a study published in the New England Journal of Medicine, CPAP is effective in reducing apnea events by 50% or more in 70-90% of patients with moderate to severe sleep apnea.
Are there any specific criteria a patient must meet to be considered for a tonsillectomy as a treatment for sleep apnea?
Yes, there are specific criteria that a patient must meet to be considered for a tonsillectomy as a treatment for sleep apnea. Generally, the main factors include having moderate to severe obstructive sleep apnea (OSA), where the blockage of the airway is primarily caused by enlarged tonsils, and previous unsuccessful attempts at non-surgical treatments like continuous positive airway pressure (CPAP). According to research studies, approximately 80% of children and 50% of adults with OSA show significant improvement or resolution of symptoms after undergoing a tonsillectomy. However, it is crucial for patients to consult with their healthcare provider for a thorough evaluation and proper diagnosis before considering this surgical option.
What are the potential risks and benefits of having a tonsillectomy for sleep apnea?
The potential benefits of having a tonsillectomy for sleep apnea include improved breathing during sleep, reduced snoring, and increased energy levels. Studies have shown that approximately 75% of patients experience significant improvement in their sleep apnea symptoms after the surgery. However, risks are also involved, such as bleeding, infection, and damage to surrounding structures. These risks are relatively low, with a 2-4% overall complication rate. It is important to weigh the potential benefits against the risks and consult a medical professional for personalized advice.
How does tonsillectomy improve sleep apnea symptoms?
Tonsillectomy improves sleep apnea symptoms by removing the enlarged tonsils that block the airway during sleep. This surgery allows for better airflow, reducing or eliminating the episodes of apnea and snoring. According to a study published in The Lancet, 72% of patients who underwent tonsillectomy showed significant improvement in their sleep apnea symptoms, leading to better quality of sleep and decreased daytime fatigue.
