Understanding the Connection: Sleep Apnea Secondary to PTSD and Its Treatment
Aug 20th 2023
Witnessing the interplay between the mind and body can be fascinating. Still, it's less so when it manifests through distressing conditions such as Post-Traumatic Stress Disorder (PTSD) and sleep apnea. Emerging research suggests a strong connection between these two, with sleep apnea often developing secondary to PTSD. In this blog post, we’ll closely explore this link, expanding our understanding of how the trauma-scarred psyche can impact our physical health during sleep. More importantly, we'll address viable treatment options that promise relief from this tangled web of nighttime discomfort. This exploration offers hope for those wrestling with these issues in seemingly endless nights because securing sound sleep should not have to be a battle.
To claim sleep apnea as a secondary condition to PTSD, you must provide evidence that your sleep apnea is caused or aggravated by your service-connected PTSD. This may include documentation of a sleep study and an independent medical opinion showing the relationship between your PTSD and sleep apnea. To receive disability benefits for this condition, you must apply through the appropriate channels and meet certain eligibility requirements. You should work with a legal or advocacy group specializing in assisting veterans with disabilities claims.
Understanding Sleep Apnea and PTSD

Sleep apnea, a sleep disorder characterized by pauses in breathing or shallow breathing during sleep, can be closely linked to post-traumatic stress disorder (PTSD). While separate conditions, they often coexist and have a complex relationship. Understanding the connection between sleep apnea and PTSD is crucial for effective diagnosis and treatment.
To comprehend this connection better, let’s explore how sleep apnea and PTSD are intertwined.
Sleep apnea is often a secondary condition for PTSD, meaning that sleep apnea is caused or aggravated by PTSD. Sleep deprivation, fragmented sleep, chronic stress, and hyperarousal can worsen PTSD and sleep apnea. People with PTSD experience high anxiety, nightmares, and hypervigilance, disrupting their sleep patterns and leading to sleep apnea. On the other hand, sleep apnea can also exacerbate symptoms of PTSD, such as anxiety and irritability, due to inadequate restorative sleep.
Imagine a combat veteran who experienced traumatic events during their service. They now struggle with recurrent nightmares related to the trauma and find falling or staying asleep throughout the night challenging. As a result of poor-quality sleep due to both the sufferings and underlying sleep apnea, they wake up feeling exhausted and irritable. This cycle perpetuates the symptoms of both conditions.
While there is a direct correlation between the severity of PTSD symptoms and the risk of developing sleep apnea, it is essential to note that not all individuals with one condition will have the other. However, recognizing the potential overlap is crucial in providing comprehensive care for patients with either condition.
To address this complex connection effectively, it is recommended to have a comprehensive evaluation conducted by healthcare professionals specializing in sleep disorders and mental health. A thorough assessment may involve analyzing medical history, conducting sleep studies, and assessing symptoms related to both sleep apnea and PTSD.
Now that we have a better understanding of the relationship between sleep apnea and PTSD let’s explore the common symptoms of sleep apnea.
- Sleep apnea and PTSD often coexist and have a complex relationship, with sleep apnea being a secondary condition for PTSD. Individuals with PTSD can experience high anxiety, nightmares, and hypervigilance, leading to sleep apnea. On the other hand, sleep apnea can exacerbate symptoms of PTSD due to inadequate restorative sleep. Recognizing the potential overlap between these conditions is crucial in providing comprehensive patient care. A thorough assessment involving healthcare professionals specializing in sleep disorders and mental health is recommended to address this complex connection effectively.
Common Symptoms of Sleep Apnea
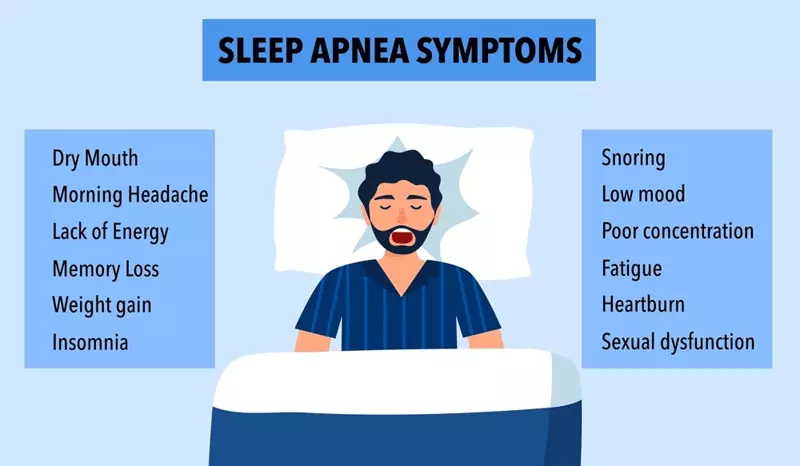
Sleep apnea can manifest in various ways, and recognizing its symptoms is crucial for early detection and intervention. Some common signs of sleep apnea include:
- Loud snoring: Frequent, loud, and disruptive snoring.
- Breathing pauses Episodes where breathing temporarily stops during sleep.
- Gasping or choking sensations: Waking up abruptly due to feelings of suffocation or choking.
- Excessive daytime sleepiness: Feeling excessively tired or falling asleep during the day.
- Morning headaches: Frequent headaches upon waking up.
- Difficulty concentrating: Experiencing problems with focus, attention, and memory.
- Irritability and mood changes: Feeling consistently irritable or experiencing sudden mood swings.
Consider a middle-aged individual who regularly snores loudly, experiences recurrent instances of gasping for breath during sleep, and wakes up exhausted despite spending enough time in bed. They struggle to concentrate on tasks throughout the day and constantly feel irritable and tired.
It is important to note that these symptoms can vary from person to person, and not everyone with sleep apnea will exhibit all of them. Additionally, some individuals may not be aware that they are experiencing these symptoms as they may not remember waking up during episodes of breathing cessation.
Recognizing the common symptoms of sleep apnea is vital as it helps individuals seek timely medical intervention and treatment options. By addressing this condition appropriately, individuals can improve their overall sleep quality and reduce the risk of exacerbating other related conditions.
PTSD and its Relationship with Sleep Apnea
Post-traumatic stress disorder (PTSD) and sleep apnea are two distinct medical conditions that can often intersect, creating complications for individuals. PTSD is a psychiatric disorder triggered by experiencing or witnessing a traumatic event, while sleep apnea is a sleep disorder characterized by pauses in breathing during sleep. The relationship between the two conditions is complex and multifaceted.
Imagine a combat veteran diagnosed with PTSD after experiencing intense trauma during their service. They may also develop sleep apnea symptoms, such as loud snoring, gasping for breath during sleep, or excessive daytime fatigue. These symptoms can be attributed to both the physical and psychological impacts of PTSD.
The connection between PTSD and sleep apnea can be bidirectional. On the one hand, individuals with PTSD may have an increased risk of developing sleep apnea due to various factors. For example, the hyperarousal state associated with PTSD can disrupt normal sleeping patterns and lead to fragmented sleep, increasing the likelihood of sleep apnea episodes. Additionally, individuals with PTSD may experience chronic stress, which can further contribute to the development or exacerbation of sleep apnea.
On the other hand, sleep apnea itself can worsen symptoms of PTSD. Sleep disturbances caused by sleep apnea can lead to increased irritability, difficulty concentrating, and heightened anxiety, all of which are hallmark symptoms of PTSD. This vicious cycle between the two conditions can significantly impact an individual's overall well-being and quality of life.
Understanding the connection between PTSD and sleep apnea is crucial for effective treatment. By addressing both conditions simultaneously, healthcare professionals can provide comprehensive care that considers the interplay between physical and mental health. Treatment options may include therapy for managing PTSD symptoms, utilizing continuous positive airway pressure (CPAP) machines to alleviate sleep apnea symptoms, or combining various approaches tailored to the individual's specific needs.
Now that we have explored the relationship between PTSD and sleep apnea let;s delve into the causes and risk factors of sleep apnea secondary to PTSD.
- According to research studies, as many as 69% of veterans receiving healthcare for PTSD screen positive for sleep apnea.
- Clinical studies reveal that 50%-90% of persons with PTSD have insomnia, and it's been noted that chronic insomnia often worsens other symptoms of PTSD, including sleep apnea.
- A study published in 2015 found a substantial overlap between PTSD and obstructive sleep apnea, with estimates suggesting that up to 58% of people with PTSD also struggle with sleep apnea.
Causes and Risk Factors of Sleep Apnea Secondary to PTSD
Sleep apnea can be a secondary condition to PTSD, meaning that it is caused or aggravated by the underlying psychiatric disorder. Several factors contribute to the development of sleep apnea in individuals with PTSD.
One significant risk factor is sleep deprivation. People with PTSD often experience nightmares and intrusive thoughts that disrupt their sleep patterns, leading to fragmented and insufficient sleep. The lack of restorative sleep can aggravate respiratory issues during sleep, increasing the risk of sleep apnea episodes.
Chronic stress is another contributing factor. The ongoing psychological distress experienced by individuals with PTSD can result in elevated cortisol levels and adrenal gland dysregulation. This, in turn, may affect the upper airway muscles' function, leading to airflow obstruction and subsequent sleep apnea.
Hyperarousal, a hallmark symptom of PTSD that involves heightened physiological and psychological responses to perceived threats, can also play a role in sleep apnea development. The increased muscle tension and heightened sensory alertness associated with hyperarousal can lead to breathing difficulties during sleep.
Additionally, comorbidities such as obesity and substance abuse are prevalent among individuals with both PTSD and sleep apnea. These conditions can further increase the risk of developing or exacerbating sleep apnea symptoms.
Understanding these causes and risk factors is essential for effective diagnosis and treatment. By assessing an individual's history, symptoms, and potential underlying factors, healthcare professionals can develop comprehensive treatment plans that address both PTSD and its associated sleep apnea effectively.
Stress, Adrenal Functions, and Their Impact on Sleep
Stress is an inevitable part of our lives, and its effects can permeate various aspects of our well-being, including sleep. When it comes to individuals with post-traumatic stress disorder (PTSD), the impact of stress on sleep becomes even more pronounced. PTSD can disrupt the body’s natural stress response system, which involves the intricate interplay between the brain and adrenal glands.
During periods of stress, such as experiencing a traumatic event or living with the consequences of PTSD, the adrenal glands release cortisol. This hormone helps regulate the body’s response to stress. Cortisol levels typically follow a natural daily pattern, highest in the morning and gradually decreasing throughout the day. However, individuals with PTSD often experience dysregulation in this pattern.
When someone is constantly under stress or has experienced trauma, it can lead to hyperarousal and heightened cortisol levels during nighttime. This disruption in cortisol secretion interferes with normal sleep architecture and can contribute to symptoms of insomnia and fragmented sleep for those with PTSD.
Moreover, increased cortisol levels can also affect other aspects of sleep. For instance, it may suppress delta wave sleep (deep sleep) and affect REM (rapid eye movement) sleep, which is crucial for memory consolidation and emotional regulation. Consequently, individuals may wake up feeling unrefreshed and struggle with nightmares or vivid dreams associated with PTSD.
Think of it like having a car engine constantly revving in high gear without a chance to cool down properly. Eventually, this sustained high level of activity takes its toll on the body’s systems, including the ability to achieve restful sleep.
Understanding the connection between stress, adrenal functions, and sleep is vital in addressing sleep apnea secondary to PTSD effectively. By focusing on managing stress levels and supporting healthy adrenal function, we can target the root causes of sleep disturbances in individuals with PTSD.
Now that we have explored the impact of stress and adrenal functions on sleep let’s shift our focus to treatment approaches for sleep apnea secondary to PTSD.
Treatment Approaches for Sleep Apnea Secondary to PTSD

Treating sleep apnea secondary to PTSD requires a comprehensive approach that takes into account both the underlying conditions. Since this condition involves two distinct components - sleep apnea and PTSD - treatment should target each aspect individually while ensuring they complement each other for optimal outcomes.
| Medication Therapy | Continuous Positive Airway Pressure (CPAP) | Behavioral Therapies |
|---|---|---|
| Certain medications may be prescribed to manage specific symptoms associated with PTSD and sleep apnea. These may include medications for anxiety, depression, or nightmares. For example, prazosin can help reduce nightmares and improve overall sleep quality in individuals with PTSD. | CPAP therapy is commonly used as the primary treatment for sleep apnea, including when it coexists with PTSD. This therapy involves wearing a mask over the nose or mouth during sleep, delivering a continuous flow of pressurized air to keep the airways open. By preventing interruptions in airflow during sleep, CPAP can mitigate the symptoms of sleep apnea effectively. | Behavioral therapies such as cognitive-behavioral therapy for insomnia (CBT-I) can be highly beneficial in managing both sleep apnea and PTSD-related symptoms. CBT-I focuses on addressing distorted thoughts and behaviors related to sleep while implementing techniques like relaxation training and stimulus control for better sleep habits. |
A tailored treatment plan that combines medication therapy, CPAP, and behavioral therapies offers a comprehensive approach to addressing both conditions simultaneously. By targeting the root causes and providing support from different angles, we can maximize the chances of restoring restful sleep and enhancing overall well-being.
Having discussed treatment approaches, it's important to note that the field of sleep medicine is continuously evolving, and ongoing research is dedicated to finding more effective solutions. Now, let's explore the significance of clinical trials and ongoing studies in the realm of sleep disorders secondary to PTSD.
Medications and Lifestyle Modifications
Medications for Sleep Apnea Treatment
Medications play a limited role in directly treating sleep apnea itself. However, they can be prescribed to manage related symptoms or conditions that might exacerbate sleep apnea and PTSD. For instance, if you have coexisting insomnia or anxiety disorders, your healthcare provider might prescribe medications such as benzodiazepines or selective serotonin reuptake inhibitors (SSRIs) to address these issues. While these medications can alleviate certain symptoms and improve overall well-being, it’s important to note that they do not cure sleep apnea nor are they a substitute for other mainstay treatments.
Lifestyle Modifications for Sleep Apnea and PTSD
Lifestyle modifications encompass various changes that can improve the symptoms of both sleep apnea and PTSD. One crucial factor is weight management. Obesity is often associated with an increased risk of sleep apnea and can exacerbate its severity. By adopting a healthy diet and incorporating regular physical activity into your routine, you might experience a reduction in sleep apnea episodes as well as improvements in overall health.
Additionally, quitting smoking and minimizing alcohol consumption can greatly benefit both conditions. Smoking irritates the airways, leading to inflammation and further narrowing of the air passages during sleep. Alcohol, on the other hand, relaxes the muscles in the throat, contributing to airway collapse during sleep. By making efforts to quit smoking and reducing alcohol intake, you may notice a decrease in sleep apnea symptoms and an improvement in quality of life.
Moreover, establishing good sleep hygiene practices is crucial for managing both sleep apnea and PTSD. This includes adhering to a regular sleep schedule, creating a comfortable sleeping environment conducive to restful sleep, avoiding stimulating activities or substances close to bedtime, and practicing relaxation techniques before bed. These lifestyle modifications can help optimize overall sleep quality and alleviate symptoms associated with both conditions.
It’s important to note that while medications and lifestyle modifications can support the treatment of sleep apnea and PTSD, they are not standalone solutions. They should be implemented in conjunction with other recommended treatments and therapies to achieve comprehensive management.
Impact of Sleep Apnea Treatment on PTSD Symptoms
When sleep apnea is effectively treated, it can have a notable impact on the symptoms of PTSD. One of the primary benefits is improved sleep quality. Sleep apnea often leads to fragmented and poor-quality sleep due to frequent interruptions in breathing throughout the night. Consequently, individuals may experience excessive daytime sleepiness, fatigue, and cognitive impairments. By utilizing appropriate treatments for sleep apnea, such as continuous positive airway pressure (CPAP) therapy or oral appliances, these disruptions can be minimized or eliminated, resulting in more restorative and uninterrupted sleep.
With improved sleep quality comes potential benefits for PTSD symptom management. Sleep disturbances are common among individuals with PTSD and can exacerbate their condition. By addressing the underlying sleep apnea, individuals may experience reduced nightmares, decreased hyperarousal during sleep, and overall improvements in mood and psychological well-being.
Furthermore, treating sleep apnea may help reduce the burden on the cardiovascular system caused by untreated sleep-disordered breathing. Sleep apnea has been associated with an increased risk of cardiovascular diseases such as hypertension, stroke, and heart failure. By effectively managing sleep apnea through appropriate treatments, individuals may potentially lower their risk of developing or worsening these comorbidities.
It’s important to remember that everyone’s response to treatment may vary, and addressing both conditions requires a multidimensional approach tailored to each individual’s specific needs.
